Cirrhosis develops after years of ongoing injury to the liver. Over time, healthy liver cells are replaced with scar tissue, which stiffens the organ and interferes with everything the liver quietly does for you every day like filtering toxins, regulating energy stores, producing proteins for blood clotting, and more.
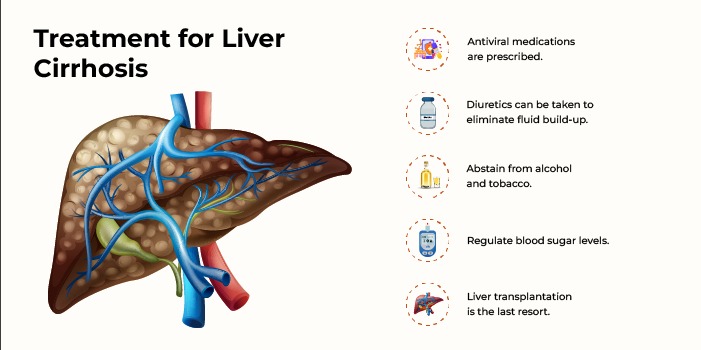
Medicines are important, but modern care is much broader than a pill bottle. It blends nutrition, procedures that lower dangerous pressures inside the liver, tools to spot problems early, and supportive therapies that help you stay active and independent for longer. If taken together and started early, these steps can slow complications and improve quality of life.
If you’re searching for Liver Cirrhosis Treatment In Ahmedabad, you’ll find that many of these approaches are available in large Indian cities with strong gastro–hepatology services and access to advanced imaging and day-care procedures. Ahmedabad’s mix of specialty clinics and tertiary centers often means shorter travel for follow-ups and easier coordination between different specialist teams that matter when treatment extends beyond medication.
It means nutrition therapy, alcohol-use treatment, targeted endoscopic or radiologic procedures (like banding or TIPS), exercise and frailty care, vaccination and infection prevention, early-warning surveillance, and in select cases microbiome or device-based therapies under research. These pieces are evidence-based and usually delivered together, not in isolation.
Elastography (ultrasound- or MRI-based) measures liver stiffness without a biopsy, helping stage disease and track change over time. Ultrasound, CT, or MRI add detail when complications are suspected.
Even when biopsy isn’t required, your team may still order it to clarify cause or severity if results are unclear. Regular surveillance imaging and blood tests also screen for varices and liver cancer in at-risk patients.
In cirrhosis, under-nutrition and muscle loss (sarcopenia) are common and directly linked to worse outcomes, so nutrition is an active treatment. Guidance from liver societies emphasizes 1.2–1.5 g/kg/day of protein, small frequent meals, a late-evening protein-rich snack, and avoiding long fasts. Managing salt (typically ~2 g sodium/day) helps control fluid buildup. When appetite is poor, fortified meals or supplements are used; a dietitian who understands cirrhosis is invaluable. Gentle resistance exercise and daily activity reduce frailty and preserve independence.
If alcohol contributed to your liver disease, structured support to stop drinking is one of the most powerful treatments available. Counselling, mutual-help groups, and, when appropriate, supervised medical therapies help maintain abstinence and reduce hospitalizations.
Sustained recovery can even allow some scarring to regress and improves eligibility for future options if needed. (Programs vary by center; ask your clinician what’s available locally.)
Endoscopic band ligation prevents or controls bleeding from enlarged veins (varices) in the esophagus or stomach. If pressure remains high despite best care, transjugular intrahepatic portosystemic shunt (TIPS) which is a small channel placed inside the liver by an interventional radiologist can redirect blood flow, reduce ascites and variceal bleeding risk, and improve comfort. TIPS does increase the chance of hepatic encephalopathy in some people, so selection and follow-up are key.
When fluid in the abdomen (ascites) causes breathlessness or pain, large-volume paracentesis (a day-care drainage procedure) provides fast relief. In people needing repeated taps, TIPS can reduce how often fluid reaccumulates and may lower the risk of kidney complications compared with ongoing paracentesis but the choice is individualized.
Infections strain a cirrhotic liver and can trigger sudden worsening. Vaccination against influenza, pneumococcus, and hepatitis viruses, prompt antibiotics for serious infections, and hand-hygiene/food-safety habits are all part of keeping you well between clinic visits. (Your clinician will tailor your vaccine plan to your labs and prior immunizations.)
The first-line treatments for confusion from liver toxins are medications, but research is exploring the gut–liver axis. Early trials of fecal microbiota transplantation (FMT) in carefully selected patients with recurrent encephalopathy have shown fewer hospitalizations and cognitive gains, though it’s not mainstream yet and should only be done within experienced programs or clinical trials.
Many people explore Ayurveda or other traditional systems. It’s wise to discuss any herb with your clinician because evidence varies and some products have been linked to liver injury.
- Phyllanthus (Bhumyamalaki): clinical evidence in chronic hepatitis B is mixed; systematic reviews conclude that current data are insufficient to recommend routine use.
- Picrorhiza kurroa (Kutki): studies suggest hepatoprotective effects in hepatitis/fatty liver models, but robust trials in cirrhosis are lacking.
- Andrographis paniculata (Kalmegh): preclinical benefits reported, but human reports include possible liver toxicity so use only with medical supervision.
- Tinospora cordifolia (Guduchi): multiple case series have described autoimmune-like hepatitis after use; avoid unsupervised consumption.
- Boerhavia diffusa (Punarnava): traditionally used as a diuretic; human evidence for cirrhosis/ascites remains sparse.
Cirrhosis raises the risk of liver cancer (HCC) and variceal bleeding. Ultrasound-based HCC screening every 6 months (with or without AFP blood test, depending on your center) and scheduled endoscopies to look for varices allow preventive banding before bleeding happens. Think of these as proactive treatments that buy time and safety.
Transplant is reserved for advanced, life-threatening disease when other measures can’t control complications. Evaluation weighs medical need, expected benefit, and readiness for lifelong care after surgery. For those with alcohol-related disease, many programs now assess candidacy individually, focusing on sustained recovery and social support. (Policies differ by center and region.)
Sometimes, if the cause is removed and scarring isn’t advanced. Alcohol abstinence, weight loss for MASLD, and controlling viral hepatitis can stabilize or even partially reverse early fibrosis in some people. Regular monitoring checks that you’re moving in the right direction.
Most people need 1.2–1.5 g of protein per kilogram of body weight daily, split across small meals with a late-evening snack to protect muscle. Plant-forward diets work well; include dairy, legumes, eggs, fish, or lean meats as tolerated.
Yes, gently and safely. Short walks and light resistance training are encouraged; avoid heavy lifting or straining when fluid is tense. Your clinician can adjust diuretics and salt limits so you feel comfortable moving.
Observational studies suggest regular coffee drinkers have lower odds of significant fibrosis and cirrhosis progression. If you tolerate it and your clinician agrees, 2–3 cups/day is reasonable. Don’t use coffee to replace medical care.
FMT is being studied for people with recurrent hepatic encephalopathy. Early trials show fewer hospitalizations and improved thinking, but it’s still specialized and not routine. Ask about clinical trials in your region.
Proceed with caution. Some herbs have limited supportive data, while others (for example, Tinospora cordifolia) have been linked to drug-induced liver injury. Always discuss supplements with your clinician and get regular blood tests if you choose to use them.
Typically every six months with ultrasound, with or without a blood test for AFP depending on local protocols. Consistent screening catches cancers earlier, when more options exist.
Not necessarily. Many people live for years with compensated cirrhosis using the approaches above. Transplant is considered when complications can’t be controlled or quality of life is severely affected despite best care.
Cirrhosis care is most effective when it goes beyond prescriptions and becomes a coordinated plan. You can live with nutrition that protects muscle, activity that fights frailty, endoscopic or radiologic procedures that prevent emergencies, vaccines and infection control, and steady surveillance to catch problems early.
If alcohol or viral hepatitis played a role, treating those causes changes the trajectory more than any single drug. Some newer options from microbiome-based strategies to antifibrosis trials are emerging, but the biggest gains still come from getting the fundamentals right and starting them early. Work with your clinician to build a simple, sustainable routine, ask which services are available close to you, and keep every follow-up.